Heart-related symptoms can be subtle, misleading, or even absent despite underlying conditions. While an electrocardiogram (EKG) remains a go-to tool for early cardiac evaluation, it often fails to detect deeper structural or coronary issues, especially in high-risk individuals. This limitation becomes especially concerning when symptoms persist or escalate, prompting the need for more definitive testing, such as cardiac catheterization.
Dr. Jose Jacob stresses that clinicians must be alert to the signs, as non-invasive tools may not be enough, and should weigh a patient’s history, risk factors, and clinical presentation carefully. Early and accurate diagnosis can lead to timely interventions, potentially preventing serious cardiac events. Careful use of available diagnostic tools, combined with strong provider coordination and modern guidelines, ensures that no warning sign goes unheeded.
EKG and Its Diagnostic Boundaries
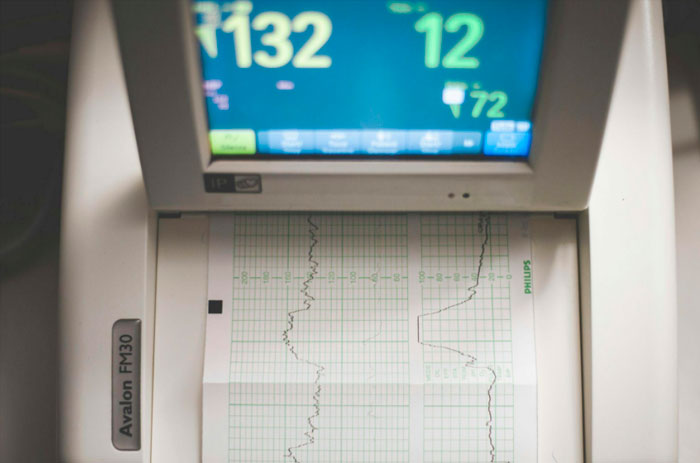
An electrocardiogram (EKG) remains a standard tool for evaluating heart rhythm and identifying acute cardiac issues such as arrhythmias or signs of a recent heart attack. It records the electrical activity of the heart and provides quick, non-invasive insight during initial evaluations. Emergency departments and clinics frequently rely on it as a first-line diagnostic tool.
Despite its utility, the EKG has limitations. Many structural heart conditions or early-stage coronary artery disease may not produce clear abnormalities on the tracing. A patient with ongoing chest discomfort could have a normal EKG while still harboring arterial blockages. Some of the most serious coronary events occur in people whose previous EKGs appeared entirely normal.
In such cases, relying solely on EKG results may delay further testing. A person with long-standing risk factors and subtle symptoms might not show any immediate electrical changes, making it important to understand where the EKG ends and other diagnostic tools begin. This awareness can be the difference between reassurance and appropriate escalation of care.
When Non-Invasive Testing Falls Short
While non-invasive tests like EKGs, stress tests, and echocardiograms provide valuable information, they don’t always reveal the full picture. In patients with ongoing symptoms but inconclusive results, diagnostic cardiac catheterization offers a more definitive assessment by directly visualizing the coronary arteries. These tests can sometimes give false reassurance when the underlying issue is mechanical or anatomical in nature.
This minimally invasive procedure involves threading a thin tube through the blood vessels to the heart, allowing physicians to detect blockages, assess blood flow, and even intervene if necessary. Someone with exertional chest pain and a normal stress test might still have significant coronary artery narrowing that only becomes apparent through catheterization.
Knowing when to move beyond surface-level tests is critical. Non-invasive tools often serve as a first step, but when symptoms persist or clinical suspicion remains high, a more direct look at the heart’s anatomy can be the difference between early treatment and missed diagnosis. The decision to escalate should never rely solely on one test result when patient symptoms tell a different story.
Symptoms That May Require Further Evaluation
Not all heart conditions reveal themselves. A person may report pressure in the chest, shortness of breath during routine activity, or even episodes of fainting, yet their initial tests—including EKG—return unremarkable findings. These red flags shouldn’t be dismissed. Symptoms can be intermittent or masked by other conditions, making them harder to interpret.
In certain cases, stress testing or imaging may hint at underlying disease without confirming its severity. If a patient’s symptoms don’t align with non-invasive findings, additional evaluation through cardiac catheterization can uncover critical information that changes the course of care. Even subtle, recurring symptoms in high-risk individuals can signal the need for further investigation. A sharp clinical eye is vital in piecing together these diagnostic puzzles.
Identifying High-Risk Patients
Certain individuals carry a higher likelihood of developing coronary artery disease due to well-established risk factors such as diabetes, high blood pressure, smoking habits, and a strong family history. These patients often require closer monitoring and earlier access to advanced cardiac testing. The presence of multiple risk factors compounds the chance of silent disease progression.
In clinical settings, it’s not uncommon to see someone with minimal symptoms but a heavy risk profile who ends up having significant arterial blockage. Traditional testing might not always raise alarms, yet their underlying vulnerability warrants more aggressive evaluation. A proactive mindset can prevent a catastrophic first event.
Recognizing these patterns helps guide timely referrals and avoids waiting for more obvious symptoms to appear. In populations where heart disease is more prevalent, proactive care can dramatically alter outcomes. The cost of waiting can be far greater than the cost of early intervention.
Coordinating Care for Timely Diagnosis
Primary care providers are often the first to detect subtle signs that something may be wrong with the heart. Their role in initiating further evaluation and coordinating with cardiology is essential for ensuring patients receive appropriate care without unnecessary delays.
When communication between providers is streamlined, patients benefit from faster diagnosis and treatment. A general practitioner noticing recurring complaints of fatigue or breathlessness may decide to consult a cardiologist even in the absence of alarming test results. That judgment call can lead to life-saving interventions when more invasive studies reveal hidden diseases. Seamless coordination also builds patient trust and improves adherence to recommended care.
Weighing Risks and Benefits
Cardiac catheterization, while more invasive than other tests, can offer life-altering clarity when used appropriately. Catching disease early allows for interventions that prevent heart attacks or worsening heart function. The ability to diagnose and treat in the same procedure often outweighs potential risks. In skilled hands, the process is quick and well-tolerated.
Though the procedure involves some degree of risk, complications are rare and increasingly well-managed. Advances in imaging technology and evidence-based referral criteria have improved the safety profile and accuracy.
